sepsis explained
Sepsis is the body’s life-threatening inflammatory response to an infection that can damage its own tissues and organs. Sepsis is a time-critical emergency that can lead to shock and potentially death if not recognised early and not treated promptly.
Sepsis is not blood poisoning or septicaemia (these are infections in the blood) but is instead the body’s REACTION to the infection that is not controlled and needs urgent treatment (antibiotics) to stop the reaction.
Sepsis is a serious illness that is very difficult to recognise, diagnose and treat. Up to 50% of sepsis survivors have long terms and in some cases life-long consequences. Time is critical so if you or someone you know is feeling really unwell and not sure why then contact a health professional or go to the closest emergency department and always ask…”could it be sepsis?”
Spotlight on sepsis | Consumer video
Over 80% of sepsis cases start in the community. This video provides information about sepsis, its signs and symptoms and potential health problems after sepsis. By raising awareness among the general public, health consumers can be empowered to speak up to clinicians about sepsis. Just ask: Could it be sepsis?
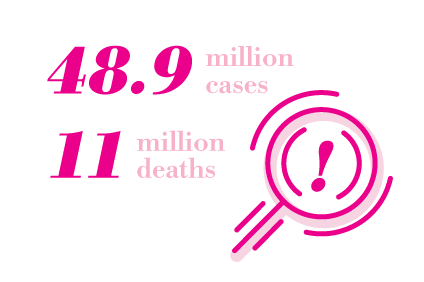
Magnitude of the problem
Sepsis is the leading cause of death from infection around the world and in Australia affects 84,000 people each year, of which 12,000 will die, three times more than common cancers, and four times more than road trauma. Sepsis affects people of all ages and patients across a broad range of clinical specialties but particularly the very young, the very old and Aboriginal and Torres Strait Islander peoples. Despite advances in modern medicine like vaccines, antibiotics, and acute care, millions of people around the world (1 in 5) die of sepsis every year and the incidence of severe sepsis continues to increase both in Australia and in other countries leaving more survivors with long-term chronic poor health or life long disability.

Causes and Prevention
Sepsis is generally associated with infections acquired in hospital, however 80% of cases occur in the community. Any infection can trigger sepsis in any person if they are predisposed to an uncontrolled hyper-inflammatory response but why this occurs in some people and not others is not well understood. Infections can be viral (e.g. COVID, RSV), bacterial (e.g. Staphylococcus Aureus, Streptococcal), fungal or many other microbes. Infection may arise in the lungs, urinary tract, skin, abdomen or other part of the body through cross infection in the air or fluids or food, injury that can be even very minor, soft tissue injury and surgery.
Preventing sepsis involves getting vaccinated against infections like flu and pneumonia, practicing good hygiene and wound care, seeking prompt medical treatment for infections, managing chronic conditions effectively, and recognising symptoms early. Be sepsis aware and educate your friends and family.
Early sepsis is difficult to recognise and sufferers may look generally unwell but it can rapidly escalate to critical illness. If you or a loved one is unwell, feel worse than when previously ill, are showing some change in one or more signs of sepsis and you’re concerned, then trust your intuition and TAKE ACTION quickly to seek advice from Health Direct or go immediately to the closest Emergency Department/Urgent Care Centre or call 000 for an Ambulance and always ask…could it be sepsis?
People at Risk
Anyone can develop sepsis, but children, infants, the elderly, and people with weakened immune systems are most vulnerable. People with chronic illnesses, such as diabetes, AIDS, cancer and kidney or liver disease are also at increased risk, people without a functioning spleen, severe burn or physical trauma. Sepsis survivors are also more at risk to have a sepsis reaction to infection though the reason for this is not fully understood and research is investigating why and how to prevent reoccurrence and readmission to hospital.
Signs and Symptoms
Sepsis is treatable if caught early. It can occur as a result of any infection, so it is important to be aware of sepsis symptoms. It may not be a single symptom but a combination of changes in the following symptoms and feeling worse than usual, when generally unwell with no obvious reason:
- rapid breathing
- rapid heart rate
- confusion, slurred speech or disorientation
- fever or shivering
- muscle pain
- not passing urine
- discoloured skin
Sepsis can deteriorate more rapidly in young children and infants. It may not be a single symptom but a combination of changes in symptoms and your concern you child is looking or feeling worse than usual, when generally unwell with no obvious reason. Seek urgent medical care if your child has:
- convulsions or fits
- rapid breathing
- discoloured skin, very pale or bluish
- a rash that doesn’t fade when you press it
- fever OR very low temperature
- not passing urine (or no wet nappy) for several hours
- vomiting repeatedly
- not feeding
If you or your child have any of the symptoms listed and are concerned, seek medical help and call 000 if a sudden change occurs. Importantly, If you have been reviewed by a Doctor or Nurse and sent home but you or your child is not improving, and you are concerned then return immediately to the Emergency Department and ask, “could it be sepsis?”

Treatment
Confusion surrounds the overuse of antibiotics in sepsis. Never delay the administration of antibiotics if sepsis is suspected. Good antimicrobial stewardship should be practiced by all health professionals meaning that after administration, the antibiotic can be changed or specifically tailored to the infection or ceased completely, based on the results of the tests taken to isolate the organism.
Recovery
Many people who survive severe sepsis recover completely and their lives return to normal. But some people, especially those who had pre-existing chronic diseases, may experience permanent organ damage. For example, in someone who already has kidney impairment, sepsis can lead to kidney failure that requires lifelong dialysis. Patients who have the extremely severe septic shock may develop gangrene necessitating the amputation of digits (fingers or toes) or even partial or complete amputation of limbs. Other patients who have not experienced the most catastrophic complications of sepsis may still feel their longer-term health has suffered as a result of contracting sepsis. Increasingly Doctors, Nurses and Allied Health workers recognise that this represents a post-sepsis syndrome, the common problems that afflict those who have recovered from sepsis have been termed the post-sepsis syndrome.
resources
A National Sepsis Data Plan – Strategic AnalysisReport
Sepsis Australia in partnership with the Australian Commission on Safety and Quality in Healthcare and…
Sepsis information for parents, carers and families of children who have died from sepsis – QLD Paediatric Program
For more information visit: Children’s Health Queensland
Sepsis Spotlight December
Welcome to the December 2025 Edition of Sepsis Spotlight! Thank you for your continued commitment…
Faces of Sepsis
SHARE YOUR STORY
If you have been affected by sepsis, we’d like to hear from you.
Frequently asked questions
These are the answers to some of the most common questions we receive about sepsis
Sepsis is an illness that can happen in response to an infection and can quickly become life-threatening. It can affect all parts of the body. In severe cases of sepsis, one or more organs fail. In the worst cases (known as septic shock), sepsis causes the blood pressure to decrease to dangerous levels and the heart to become weaker. Once this happens, multiple organs may fail quickly and, if not corrected, the patient will die. Sepsis is a medical emergency that can be difficult to diagnose, and to treat.
Common symptoms of sepsis are fever, chills, rapid breathing, rapid heart rate, rashes, drowsiness, confusion, and disorientation, and not passing urine. Many of these symptoms, such as fever and difficulty with breathing, are similar to symptoms of other conditions, like the flu. This makes it difficult to diagnose sepsis in its early stages, especially in hospitalised patients who will have other causes of those symptoms.
Sepsis occurs when the body’s response to an infection becomes harmful. Infection causes your immune system to release hormones, enzymes, proteins and other chemicals to fight the infection. These chemicals can cause generalised inflammation in the body making blood vessels leak and causing blood clots. These changes can damage all the body’s organs. Almost any type of infections can lead to sepsis, this includes infections of the lungs, abdomen (such as appendicitis), urinary tract, skin, or other part of the body. Infections acquired in hospitals or other healthcare settings (healthcare-associated infections), can also lead to sepsis.
Common related conditions include Meningococcal disease, influenza and COVID, and Group A Streptococcus, a bacterium that can cause many different infections including Strep throat, Scarlet fever, Impetigo, Pneumonia, Necrotizing fasciitis, Otitis media (ear infections), Sinusitis, Cellulitis for cuts and ulcers, and toxic shock syndrome
Anyone can get sepsis, but the risk is higher in:
- Infants and young children
- Maternal women
- Elderly people
- First Nations people
- People with weak immune systems and pre-existing illness, such as diabetes, AIDS, cancer, and kidney or liver disease, or physical trauma
Each year around 84,000 people suffer sepsis of which 12,000 will die and up to 50% experience long-term to lifelong complications and the incidence is increasing.
There is no single test for sepsis. If suspected or concerned treatment with antibiotics must start immediately. Doctors will suspect sepsis from a number of physical symptoms like fever, increased heart rate, increased breathing, mental confusion or drowsiness. They will also take blood, urine and other samples to send to the laboratory for testing ideally before antibiotics are given but this should never delay antibiotic administration if there is difficulty obtaining the samples. Once results are received antibiotic therapy is modified or ceased accordingly. X-ray and scans may be performed to identify or confirm the source of the infection.
People with sepsis are treated in hospital and those with severe sepsis are usually treated in the intensive care unit. Treatment targets the infection, while supporting vital organs and giving intravenous fluids and drugs to maintain blood pressure. In severe cases when organs fail, life-support treatments such as artificial ventilation (breathing machine) or kidney dialysis, may be necessary. Surgery may be needed to control a local site of infection such as in appendicitis or following a perforated bowel.
Many people who survive severe sepsis recover completely and return to normal lives. Some people, especially those who have required prolonged treatment in an ICU may experience longer term problems including permanent organ damage. Other longer-term effects include difficulty sleeping, concentrating or returning to work, reduced energy and musculoskeletal problems. Each person’s reaction to sepsis is individual due to underlying risks, lifestyle, environment and vaccination status.
make a difference and join us today in the fight against sepsis
Together, we can raise awareness, improve care, drive research and save lives.




